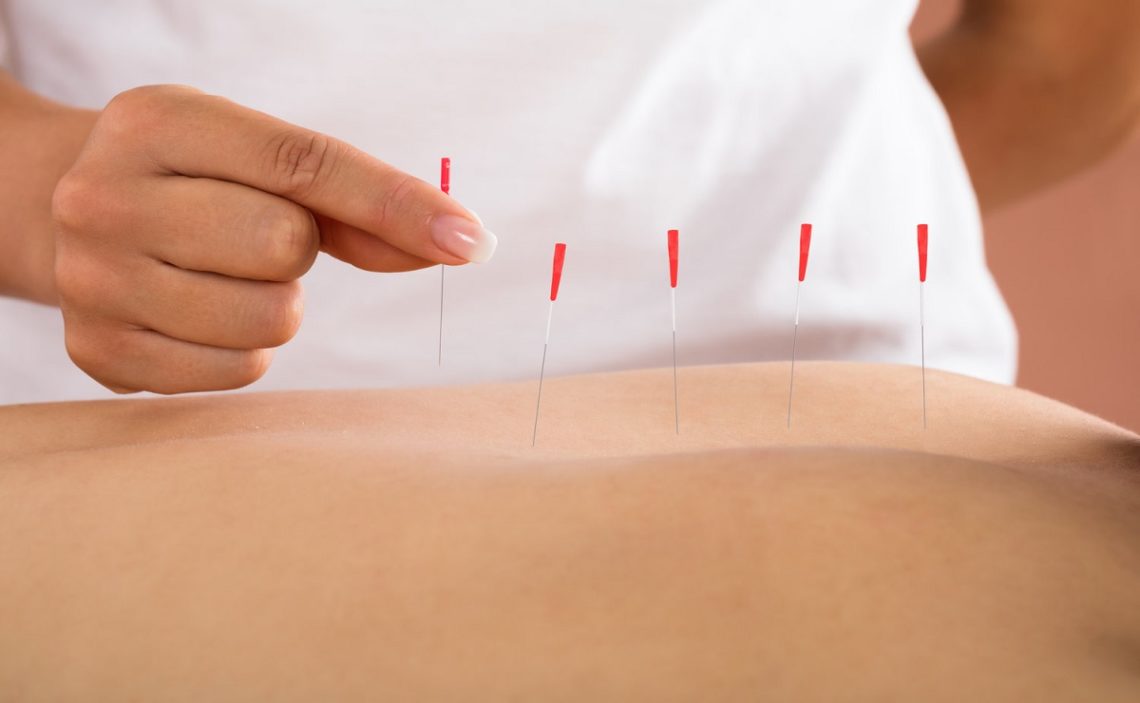
In physical therapy settings, the use of dry needling to reduce pain and improve patients’ range of motion has increased recently. Tiny needles are inserted through the skin and into the muscle at designated trigger points to elicit a contraction reflex.
It is generally a safe procedure. However, there can be problems, as with any treatment. One of the common questions from patients, in addition to possible complications, is whether they can include these bills in their insurance.
Does my insurance pay for dry needling?
Despite overwhelming evidence, many U.S. insurance companies, including CMS and Medicare, refuse to cover dry needling because they consider it experimental or investigational.
In demanding it, one insurer has gone further, stating that “patients must be informed in writing that there is conflicting evidence on the efficacy of dry needling, that the therapy is unproven, and that it is therefore not a covered service.”
All procedures, including those without an established history, should be noted in the patient’s medical record and a statement of their unproven status. They even published a “Clinical Practice Guideline on Dry Needling Policy.”
It is fascinating to consider the motivations behind the choice of commercial or private insurance companies to deny coverage for dry needling.
Because in 2019, the average annual premium for a family was more than $20,000, and the average annual premium for individual coverage was more than $7,100, according to a Henry J. Kaiser Family Foundation survey.
Over the past five years, premium costs have increased by 22%, and over the past ten years, by 54%. The goal of an insurance company is to maximize profits. Employers and individual policyholders contribute underwriting capital to the insurance company.
All customer payments are used to cover operating expenses and health care claims. One would assume that, given the types of premiums charged by the insurance companies, they would be sufficient to pay all medical claims.
What is the price of dry needling?
The typical cost per session is between $35 and $85. Depending on your problem or injury and overall physical therapy needs, the initial evaluation may cost more.
A typical dry needling therapy session may include additional components, which drives up the cost. It may include typical physical therapy exercises, electrical stimulation, muscle massage, and joint manipulation.
Risks associated with dry needling
There may be a greater likelihood of malpractice and errors during a dry needling session because there is less supervision by dry needling practitioners. Infections or injuries to tissues and nerves may happen due to sterile or improperly inserted needles.
While a well-managed session can be expected to cause some mild discomfort at the insertion site, patients should be aware of any therapy that causes severe or prolonged pain.
Few studies, considered inconclusive, examine the effect of dry needling in reducing muscle pain and other symptoms. In addition, client testimonials are inconsistent.
Further research is needed to provide a better context for clients, and practitioners believe this process can yield results. It is a relatively new practice with an experimental theory.
Does Medicare cover the treatment?
Dry needling procedures are not currently covered by the original Medicare insurance, resulting from the lack of study of the practice and the lack of regulation of its practitioners.
You may want to check with your plan for details on whether alternative therapies such as dry needling are covered because private Part C insurers that provide Medicare Advantage plans may offer additional benefits.
Medicaid often covers many services not covered by Original Medicare for those who are dually entitled to coverage through both programs. However, dry needling is not currently accepted by Medicaid.
Beneficiaries should continue to evaluate their policies for modifications that may include services that were not covered in the prior year, and conditions of coverage are subject to change annually.