Under the Affordable Care Act, insurance plans must offer free patient-paid coverage for several preventive treatments, including colonoscopies. However, the insurance industry has imposed strict requirements on what constitutes a preventive service.
According to guidelines, the definition of preventive colonoscopy cannot be met by patients with symptoms, a history of gastrointestinal disease, or a personal or family history of colon polyps or colon cancer.
Does insurance cover the colonoscopy kit?
The most expensive screening test available to Americans is colonoscopy. According to data, more than 10 million Americans are screened for colon cancer each year, collectively spending $10 billion on colonoscopies alone.
The U.S. Preventive Services Task Force (USPSTF) strongly advises that all Americans undergo proactive colonoscopies to reduce the death rate from colon cancer.
A federal law was passed that reduces the out-of-pocket costs of colonoscopy to encourage more people to undergo colorectal cancer screening.
Whether colonoscopies are performed as normal screening procedures or to identify a potential problem, Medicare will pay for them. Depending on the reason for the surgery, the insurance company will decide whether to pay for the procedure.
Under Part B of Original Medicare, screening and diagnostic colonoscopies are covered. If you are at high risk for colorectal cancer, you are offered a free screening test every 24 months. Medicare will pay for the screening test in full once every ten years if you are not at high risk.
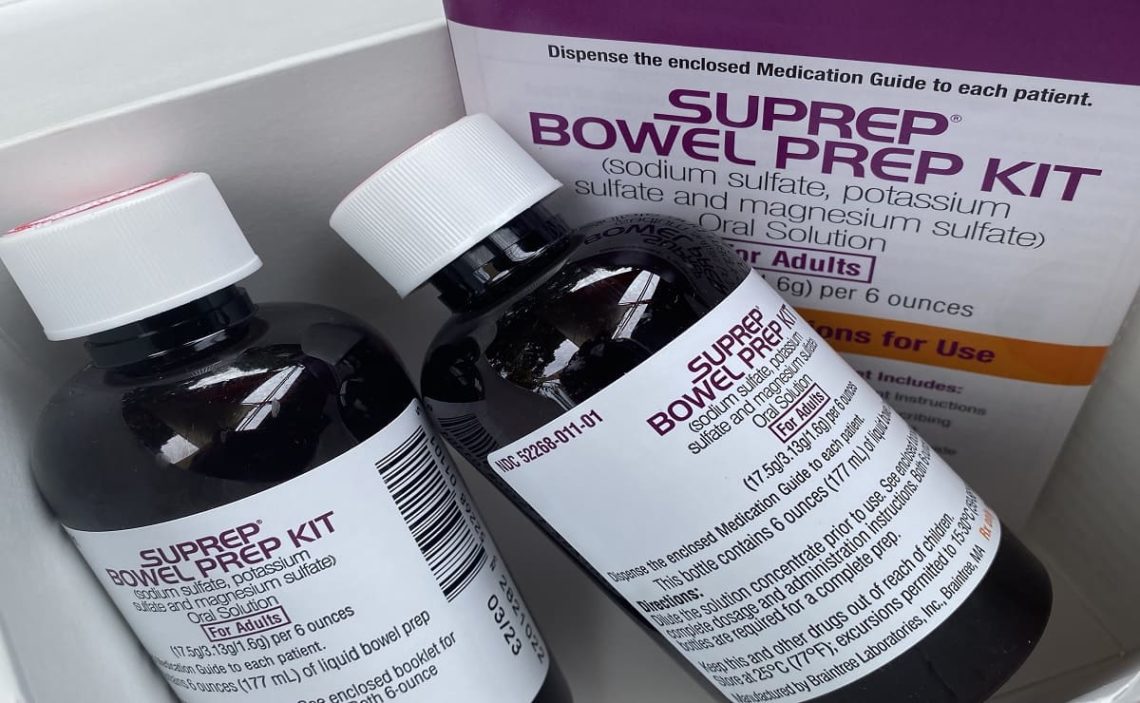
The prep kit
Your doctor will probably prescribe a prep kit in liquid or pill form if you are advised to have a colonoscopy. Thanks to this prep kit, you can help the doctor perform the colonoscopy by cleansing your digestive system.
The colonoscopy prep kit should be dispensed at a pharmacy and charged to your Part D drug plan if your doctor prescribes it. Colonoscopy prep kits are not covered under Part B. The number of colonoscopy prep kits covered by your plan depends on your Part D prescription drug plan’s insurance coverage.
What if you don’t have insurance?
Colon cancer screening is necessary, but for those without insurance, it’s harder to get. However, there are ways to get a colonoscopy at little to no cost. New Yorkers between the ages of 50 and 75 who are uninsured can get a colon cancer screening through the New York State Cancer Services Program (CSP).
Another source for a free or inexpensive at-home FIT test or discounted colonoscopy is the Colorectal Cancer Alliance. FIT immunochemical testing Patients can compare colonoscopy prices at their location using the Healthcare Bluebook.
When is it time to have a colonoscopy?
Aside from skin cancer, the third most commonly diagnosed cancer in the United States in both men and women is colorectal cancer, which begins in the colon or rectum. Polyps, which are growths on the inner lining of the rectum or colon, are the precursors to most malignant colorectal tumors.
Doctors can find polyps during a colonoscopy and remove them to stop their growth. Polyps usually start tiny and can develop into cancer as they mature.
Removing the polyp before it becomes cancerous is the first advantage of a screening colonoscopy. Colonoscopies consistently beat colon cancer. Dr. Williams has affirmed the above.